By Dr. Ameya A. Asarkar, Dr. Jason Calligas, and Dr. Cherie-Ann O. Nathan
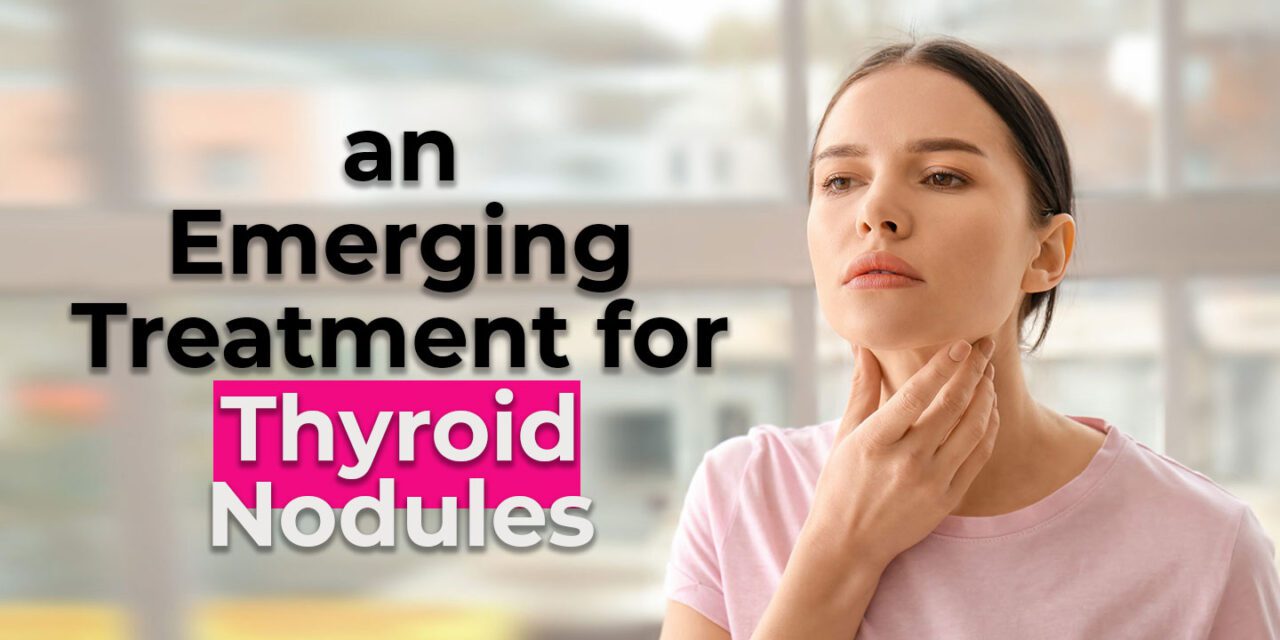
The thyroid is an endocrine gland that is small and butterfly-shaped, located at the front of the neck. This gland is responsible for controlling the speed of the body’s metabolism or metabolic rate, which is the process of how the body transforms consumed food into energy. Because the entire body relies on this process, if the thyroid isn’t working properly, it can have negative impacts on the entire body, too. The thyroid affects bodily functions such as metabolism, heart rate, breathing, digestion, body temperature, mental activity, brain development, and fertility.
A common thyroid issue that affects 20%-76% of adults is thyroid nodules. A nodule is a lump, or growth, of cells in the thyroid gland. This condition is four times more likely to affect women, and do not affect children as much as adults. With the increased use of imaging tests like the ultrasound or the CT scan, incidental thyroid nodules are being identified with increased frequency in recent years. Sometimes, these nodules may be identified during a routine primary care visit or by the patient themselves while looking in a mirror or while fastening a necklace. Most of these nodules are noncancerous or benign in nature and do not warrant intervention. While still benign, sometimes thyroid nodules may cause conditions such as hypothyroidism or hyperthyroidism.
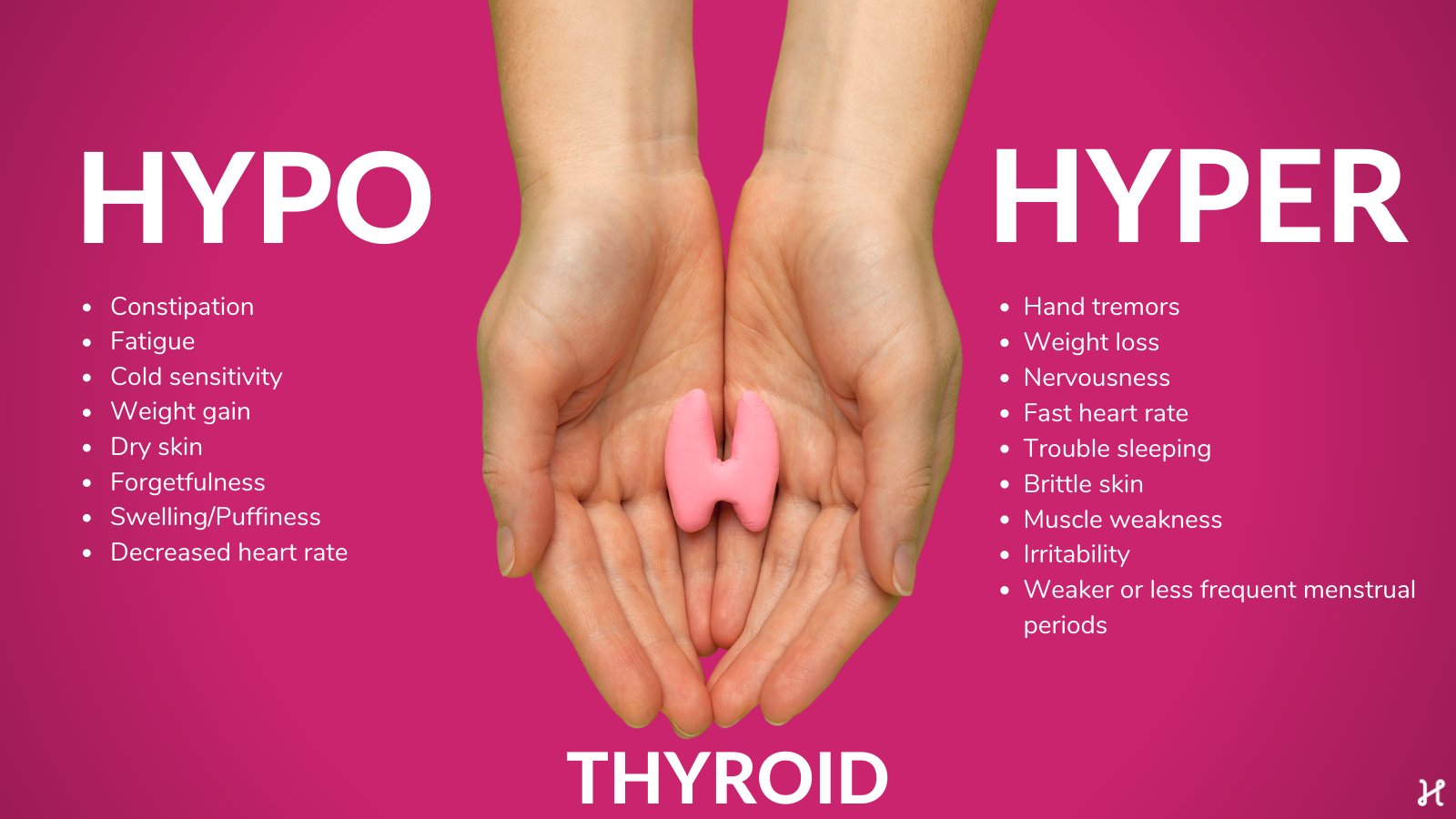
Hypothyroidism, or low thyroid hormone levels, may cause symptoms of fatigue, numbness of the hands, weight gain, dry skin, or depression, while hyperthyroidism, or overproduction of thyroid hormones, may cause symptoms of rapid heartbeat, weight loss, increased appetite, difficulty sleeping, and shakiness. These conditions are typically treated with medications.
Occasionally, benign nodules require surgical removal if they cause compressive symptoms or cosmetic deformity. A removal technique, radiofrequency ablation (RFA), has recently gained popularity as an attractive option for patients who refuse surgery or are not surgical candidates.
RFA is the process of creating thermal energy when electrical current is passed through tissue (thyroid nodule) which induces necrosis and fibrosis and eventual tissue reduction. RFA is an image guided ablative technique and uses ultrasound as the modality of choice for imaging.
RFA is performed under local anesthesia with or without sedation. Under ultrasound visualization, the RFA probe is introduced into the thyroid nodule with a ‘moving shot technique’ wherein the operator moves the RFA probe back and forth while observing the changes in the tissue on the ultrasound. The heat created raises the tissue temperatures to 60 to 100 degrees Celsius. Observing the tissue in real time helps the operator ablate the entire lesion while avoiding transmission of thermal energy to nearby structures.
Overall, RFA has lower risks when compared to surgery. Heat damage to the surrounding structures is the most common cause of complications following the RFA procedure. The ‘danger triangle’ has been described as the location of the nerve that moves the vocal cords where it is in close proximity with the wind-pipe and the thyroid gland. Studies have shown that voice changes or hoarseness are reported in less than 1% patients, and most of these patients do not require any treatment.
In one study an overall complication rate of 4.6% and a major complication rate of 1.3% in patients undergoing RFA. Few other complications of RFA include:
- Pain or discomfort
- Nausea
- Nodule rupture
- Skin burn
- Bleeding
- Needle track seeding
- Injury to nerves
- Injury to the wind-pipe or swallowing passage
Guidelines from multiple national and international head and neck surgery/endocrinology societies have been developed to guide the use of RFA for treating thyroid nodules. Confirming two benign results on a needle biopsy is recommended prior to recommending RFA. Other patients who can benefit from this procedure include patients with cosmetic concerns and want to avoid neck scars.
The role of RFA in cancerous nodules is upcoming and still an area of research. Recent studies have shown that RFA is safe in low-risk papillary thyroid carcinoma (PTMC) and does not compromise oncologic outcomes. These results, however, should be cautiously interpreted and treatment should be individualized. Without long term data, at present, RFA is not generally recommended in any other types of thyroid cancers and if used should be a multidisciplinary team decision.
Overall, RFA is an effective, safe, and minimally invasive alternative to surgery in a select group of patients. With the recent publication of the best practice recommendations from national and international thyroid societies, the use of RFA in treating thyroid nodules will become more standardized. Future studies with long term follow-ups will solidify the use of RFA as its indications are constantly evolving.