Role of ECT in Psychiatry
WHAT IS ECT?
Electroconvulsive therapy is a safe and effective treatment that involves passing a carefully controlled electrical current through a person’s brain to trigger a seizure — a rapid discharge of nerve impulses throughout the brain. In recent years, the National Institute of Mental Health, the American Psychiatric Association, and the U.S. Surgeon General all endorse ECT as a valuable tool in the treatment of certain psychiatric disorders, and treatment resistant depression in particular. Each year thousands of patients are treated with electroconvulsive therapy (ECT) in Psychiatry and Behavioral Sciences. This procedure can be done on an inpatient or outpatient basis.
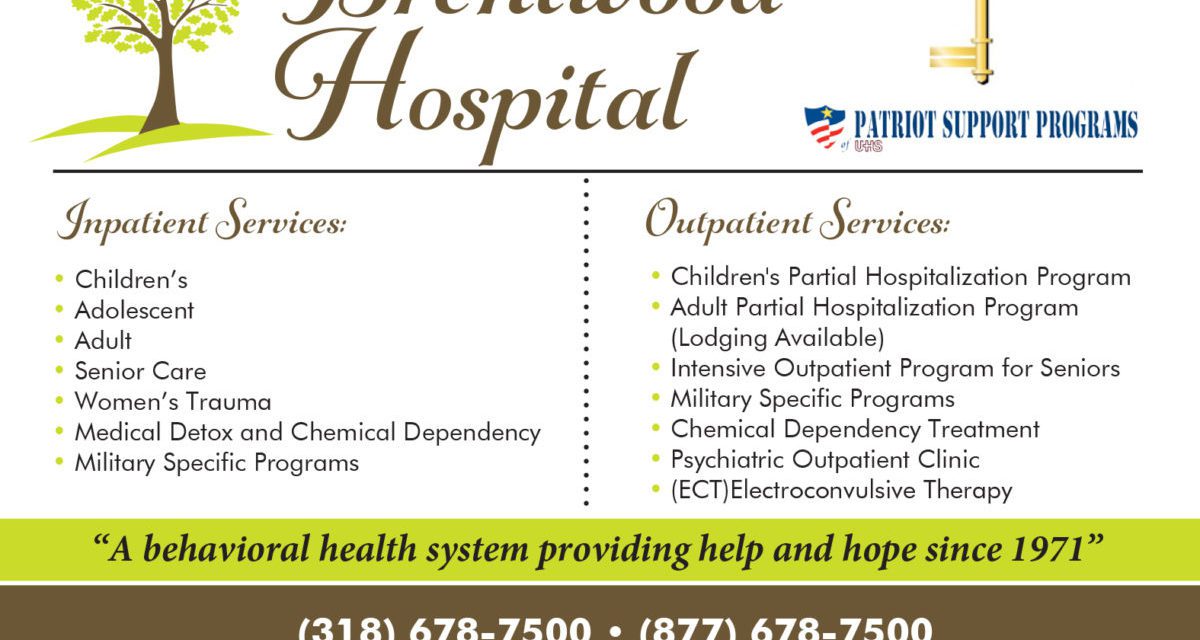
Brentwood Hospital now provides ECT treatment with ultra-brief pulses to reduce cognitive side-effects. Recent studies demonstrate that ECT delivered with ultra-brief pulses produces less memory loss and other cognitive side-effects than ECT delivered with standard pulses.
HOW DOES ECT WORK?
The exact mechanism is not known, however many studies with advancement in research over many decades show, it may promote changes in how brain cells communicate with each other at synapses and it may stimulate the development of new brain cells. ECT may flood the brain with neurotransmitters such as serotonin and dopamine, which are known to be involved in conditions like depression and schizophrenia.
WHEN IS ECT USED?
People with major depression typically first receive antidepressant medication and psychotherapy. These treatments, though often effective, take time to work. This delay can be dangerous for patients whose depression is accompanied by delusions (false beliefs) or intense suicidal thoughts. ECT can work much more quickly than antidepressants and is useful when patients are at immediate risk for self-injury or suicide.
ECT may also be prescribed when antidepressant medications have not worked. It can be useful for older patients who are unable to tolerate antidepressants and for pregnant women in whom medication might damage the fetus. People suffering from bipolar disorder and schizophrenia may also benefit from ECT.
WHAT HAPPENS DURING AN ECT PROCEDURE?
Before ECT, patients are asked not to eat or drink after midnight the night before treatment.
During the procedure, the patient receives a short acting anesthetic agent which puts the patient to sleep for approximately 5-10 minutes. A muscle relaxant is also used during the procedure to stop the patient’s muscles from moving during the seizure. Cardiac monitoring pads are placed on the patient’s chest to monitor the cardiac status during and after the procedure. Four electrodes are placed on specific areas of the patient’s head. Two of these electrodes are for monitoring the brain waves. The other two are for delivering a short, controlled set of electrical pulses for a few seconds. The electrical pulses must produce a generalized seizure to be effective. Because patients are under anesthesia and have taken muscle relaxants, they neither convulse nor feel the current.
Patients awaken about 5 to 10 minutes after the end of the treatment. Patients are then moved to the recovery room and remain there until their blood pressure, pulse and breathing return to their pre-treatment levels. Usually this takes about 20 to 25 minutes.
Patients who are given ECT on an outpatient basis must have someone drive them home after the procedure and stay with them until they go to sleep at night. People should not drive in the 24 hours following ECT.
HOW LONG IS AN ECT PROCEDURE?
A single ECT session usually lasts one hour. This includes the time the patient will be in the treatment room (approximately 15-20 minutes) and the time spent in the recovery room (approximately 20-30 minutes).
Typically, ECT (whether inpatient or outpatient) is given two to three times a week for a total of six to twelve sessions. Some patients may need more or fewer treatments.
These sessions improve depression in 70 to 90 percent of patients, a response rate much higher than that of antidepressant drugs.
Although ECT is effective, in some patients its benefits are short-lived. For this reason, patients take antidepressant medication after ECT or may continue receiving ECT periodically to prevent relapse.
WHAT ARE THE SIDE EFFECTS OF ECT?
The immediate side effects of the procedure can include headache, nausea, muscle aches and soreness, disorientation and confusion. These side effects may last about one hour.
Patients may also develop memory problems. Memories formed closer to the time of ECT are at greater risk of being lost while those formed long before ECT are at less risk of being lost. The ability to form new memories is also impaired after a course of ECT treatments, but this ability usually makes a full recovery in the weeks and months following the last treatment.
HOW CAN FAMILIES HELP PATIENTS WHO WILL BE RECEIVING ECT?
The treatment team will enlist the family’s help in assessing a patient’s progress. Families can help by providing a gentle reminder of the day and date and remind them that feeling confused is to be expected. Family members should inform the nurse of any concern they have about their loved one.
HOW DO I MAKE A REFERRAL?
Referrals can be made by physicians, psychiatrists, mental health professionals, hospitals, patients, and concerned family members. The patient will meet with the ECT coordinator to determine if he or she is an appropriate candidate for treatment.
To find out if ECT may be right for you, contact the intake department at 318-678-7500 or 877-678-7500 for an assessment.
We accept Medicare, TRICARE® and most private insurance plans.