Get ready to say goodbye and good riddance to lower back pain.
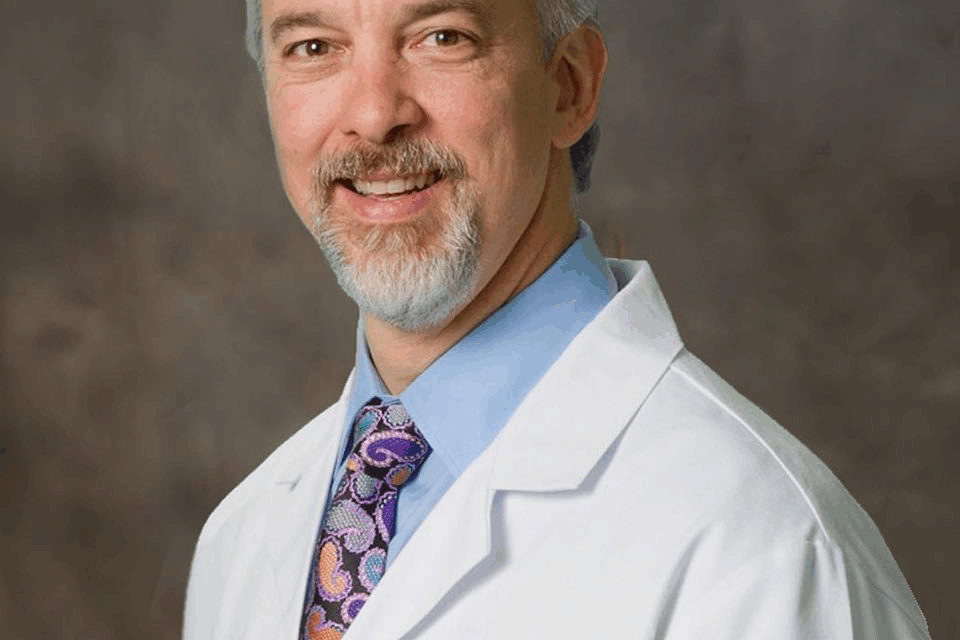
In a world driven by progress, a select group of individuals stands at the forefront of innovation, particularly in the realm of medicine. These are not just scientists or researchers, but minds of exceptional intellect, fueled by an insatiable curiosity and a profound desire to alleviate human suffering. What compels these highly intelligent individuals to dedicate their lives to the pursuit of new and innovative medical breakthroughs? Is it simply the allure of scientific discovery, or is there a deeper, more personal motivation driving their relentless pursuit of knowledge and solutions? To find the answers to these questions, one would have to climb into the brain of such an individual- let’s say a man like Dr. Pierce Nunley, the first spine surgeon in the nation to perform a spinal disc nucleus replacement procedure using the PerQdisc™ device.
Sitting in his office, surrounded by 3-D models of the spine and various disc replacement devices that Dr. Nunley has personally been involved with, it was difficult to NOT be overwhelmingly impressed with his accomplishments. Dr. Nunley’s work with the Spine Institute Foundation, a research foundation that has done over 35 FDA studies involving new spine care technologies, has been truly extraordinary. The most recent device, the PerQdisc, shows exceptional promise in the treatment of degenerative disc disease.
Dr. Nunley became involved with Spinal Stabilization Technologies’ (SST) PerQdisc program two years ago as consultant and later a principal investigator (PI) in the US IDE Clinical Investigation. The PI leads the clinical research team and together they monitor the trial participants’ health and progress while collecting important data pertaining to safety and effectiveness of the PerQdisc device. “When I first heard about this trial, it was at a spine conference in Cabo, two years ago. Dr. Marcus Stone and I are the principals at The Spine Network,” Dr. Nunley said (Dr. Marcus Stone runs the Spine Institute Foundation and now lives in Salt Lake City, Utah.) The Spine Network’s purpose is to assist companies with innovative ideas from inception through navigating the Food and Drug Administrations trial and approval process. “For the PerQdisc study, we worked through the design of the trial, all the inclusion/exclusion criteria, and the surgical approach.” After weighing the positives and negatives of various surgical approaches, it was Dr. Nunley who came up with the technique that will be used in the study.
For the FDA study, the ideal candidate is one that has single-level symptomatic degenerative disc disease. “They need to be super clean. They need to have one thing wrong with them,” said Dr. Nunley. “The scope is very narrow, and patient selection is very important. A thorough work-up must be performed in order to rule out other potential pain generators,” he added. Dr. Nunley, TSN, and SST worked diligently with the FDA for nearly 18 months to develop a study that would produce valuable data, while ensuring patient safety. The first study will evaluate five patients, gathering a tremendous amount of data to be able to assess the safety and effectiveness of the PerQdisc over time.
What makes the PerQdisc Nucleus Replacement procedure such a breakthrough in the treatment of degenerative disc disease (DDD) compared to other devices and traditional spinal fusion?
- It’s less invasive, which is a plus for the patient. Unlike a traditional disc replacement which requires the removal of the entire intervertebral disc, PerQdisc focuses on replacing only the nucleus pulposus (the gel-like center). This minimally invasive approach aims to preserve more of the natural disc anatomy, including the annulus fibrosus (the outer ring) and cartilaginous endplates.
- The PerQdisc implant is designed to provide a patient-specific, custom implant. The PerQdisc is formed within the disc space using balloon technology and a biocompatible silicone polymer. The surgical approach is from the side requiring about a one-inch incision. Dr. Nunley described the procedure as removing the center of the disc nucleus and then introducing a series of imaging balloons to assess the disc space and cavity that was created. “…is the cavity concentric? Is it even? If not, we’ll work it a little bit. Finally, the PerQdisc implant is introduced and filled with a silicone polymer”. This allows for a patient-specific, form-fitting implant that fills the void left by the removed nucleus, potentially leading to better stress distribution and stability. The patient is observed in the OR for about 15 minutes to allow the polymer to harden. It can be performed as an outpatient procedure with the instructions of not putting too much stress on the disc for the first few days. The less invasive nature of the PerQdisc procedure may lead to shorter surgery times, less blood loss, and a potentially faster recovery period compared to more extensive surgeries.
- Fusion surgery typically involves a more extensive surgical approach, often requiring bone grafts and hardware (screws, rods, plates) to stabilize the spine. The PerQdisc, as mentioned, is a minimally invasive procedure with no need for such hardware. Due to the less invasive nature, patients receiving the PerQdisc may experience a quicker recovery and return to daily activities compared to the often-lengthy recovery associated with spinal fusion.
- Motion Preservation is the most significant difference with the . Spinal fusion aims to eliminate motion at the affected segment by permanently joining two or more vertebrae. While it can relieve pain, it sacrifices natural movement and can lead to increased stress and degeneration in adjacent spinal levels (adjacent segment disease) By preserving motion at the treated level, PerQdisc has the potential to lower the incidence of adjacent segment degeneration, a known long-term complication of spinal fusion.
The PerQdisc is designed to restore and maintain disc height and thus, can better mimic the natural biomechanics, physiological motion and nerve function of the spine compared to TDR (total disc replacement), which, while motion-preserving, involves a complete disc removal and replacement with an artificial joint
The PerQdisc is indicated for patients with mild to moderate disc degeneration who are experiencing significant pain but are not yet candidates for fusion or total disc replacement, which are often reserved for later stages of disease continuum.
The PerQdisc Nucleus Replacement Device is still investigational in the United States and has not yet received FDA approval and is not yet commercially available in any region. The plan is to gain long-term efficacy and safety data gathered from clinical trials currently underway outside of the United States, in addition to the recently approved FDA IDE study, which Dr. Nunley and his team are leading in the U.S. Once all the data is submitted to the FDA it will take six to twelve months from that endpoint to be approved for a panel process. This last step requires sitting before a panel and submitting to a litany of questions, arguments and anti-arguments. “…you make your final arguments, like a trial, and then they literally vote in front of you,” Dr. Nunley explained. Before the FDA moves forward, this panel must approve the procedure by a majority vote. It will take about four years and roughly 40 million dollars from the beginning of the trials before this procedure will be made available to the U.S. market. That doesn’t include marketing the device, selling it and getting insurance companies to approve paying for the procedure. This last step shouldn’t be too difficult since the PerQdisc procedure will be less expensive than a disc replacement or a fusion by far.
Once the PerQdisc Nucleus Replacement Device is approved by the FDA, it will offer a potentially breakthrough approach to treating degenerative disc disease. One that is a less invasive, motion-preserving alternative to traditional fusion and a less extensive option compared to total disc replacement. Its custom-fit design and focus on nucleus replacement aim to restore natural disc function and potentially reduce the long-term complications associated with more invasive surgical treatments. Hopefully patients who suffer with lumbar back issues won’t have to wait too much longer. Even though it is still an investigational device, Dr. Nunley and his fellow team members are determined to see the FDA process through. Judging by the artifacts scattered throughout his office, Dr. Nunley is not one to throw in the towel when it comes to better outcomes for his patients.
About Dr. Pierce Nunley
Pierce Nunley, M.D., brings international experience to his position as the director of the Spine Institute. He received his M.D. from the University of Kansas Medical College and did his internship and residency at LSU Health Sciences Center, where he has served as a clinical instructor since 1999 and as an Assistant Professor in the Department of Orthopedic Surgery since 2006.
He completed a spine fellowship at the University of Basel in Switzerland in 1996 and at the Dallas Spine Group in 1997. Nunley also received specialized training at the Mississippi Sports Medicine Center in Jackson. Dr. Nunley is board certified by both the American Board of Orthopaedic Surgeons and by the American Board of Spine Surgery.
Dr. Nunley is a fellow of the American Academy of Orthopaedic Surgeons, serves on the research fund management committee of the North American Spine Society, is a board member of the American College of Spine Surgery and has membership in the Southern Orthopaedic Association and Louisiana State Medical Society. He serves on the board of the Spine Institute of Louisiana Foundation and Syndicom Inc. The company’s flagship product is SpineConnect, a leading collaborative innovation network for spine surgeons to collaborate on difficult and unusual cases.
He is published in numerous journals and books and has presented papers in Canada, Mexico and Italy, as well as all over the United States.