Rheumatoid arthritis (RA) affects 1.3 million Americans, representing about 1% of the US population. The Arthritis Foundation estimates that the global prevalence of RA is 0.5-1% in developed countries. RA is an autoimmune disorder and occurs when your immune system mistakenly attacks one’s own body’s tissues. This affects the lining of one’s joints, causing a painful swelling that can eventually result in bone erosion and joint deformity. Often, there is pain and swelling of the fingers as well as prolonged stiffness especially in the morning. RA develops gradually over many weeks to months. While it usually begins between ages 40 and 60, a similar disease can present in teenage children and is called Juvenile Rheumatoid Arthritis.
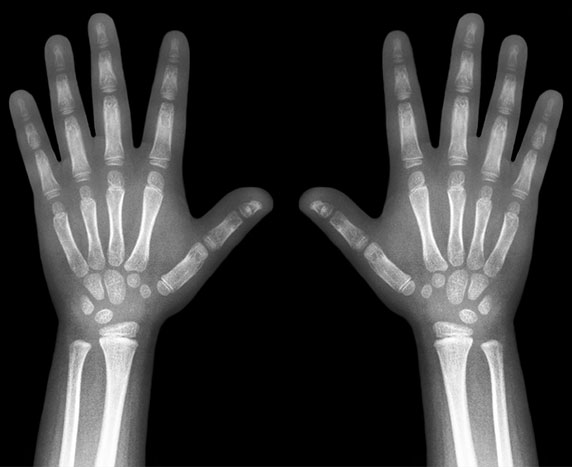
RA is diagnosed with medical history, physical examination, and blood testing. Blood testing includes markers of inflammation (Erythrocyte sedimentation rate and C reactive protein) and antibodies (Rheumatoid factor and anti-cyclic citrullinated peptide antibody). X-rays of hands and feet can show weak bones with damage, or erosions in certain areas. One must see a rheumatologist early to get RA in good control.
Treatment of RA has greatly improved during the last three decades. Initial treatment of RA includes pain medications which are not disease-modifying drugs. Another method of initial treatment includes steroids taken by mouth to control inflammation in joints in RA. Steroids are associated with many side effects with long-term use, including weak bones (osteoporosis), diabetes, high blood pressure, stomach ulcers, dead bone (avascular necrosis), increased risks of stroke and heart disease. Steroids should only be used initially in RA management for rapid response, but it is advisable to taper quickly to the lowest effective dose and stop within a few weeks.
Rheumatoid arthritis should be managed by disease-modifying anti-rheumatic drugs (DMARDs) as soon as possible to prevent irreversible damage. Usually, patients are given DMARDs like Methotrexate, Hydroxychloroquine, Sulfasalazine and leflunomide. These medications have been used for many years to control RA but have not been successful in achieving full remission (control of disease) in all patients.
The most significant improvement in RA treatment has been the discovery of biologics. Biologics target certain chemicals or cells in the immune system which are causing damage to joints. These medications have made remission (full control of disease) possible and have made a great impact on improving quality of life in RA. Physical therapy, occupational therapy, steroid injections in the joints and weight control can also have a beneficial effect on RA. There is significant interest about changing diet in RA to see improvement, and studies have shown improvement with fish oil capsules along with continued medications.
The Center of Excellence of Arthritis and Rheumatology (CEAR) at LSU Health Shreveport has been actively involved in many research projects involving use of biologics in RA. We are participating in many ongoing drug trials to discover more biologics for treatment of this chronic and disabling disease. Because of a lack of availability of good biologic medications in the past, RA patients have suffered from chronic deformities and disabilities. With the advancement of biologics treatment, the patient has full control of their disease with almost no irreversible damage to their joints. These are fascinating and encouraging times for patients and rheumatologists, as this treatment has had excellent clinical response.
If you or a loved one is experiencing these joint symptoms, consult with your doctor as soon as possible, and you may request a rheumatology referral. An early referral to a specialist is key to prevent irreversible joint damage and control the disease with prompt management.
Sarwat Umer, MD, is an Associate Program Director of the Rheumatology Fellowship with the Center of Excellence for Arthritis and Rheumatology and a Professor of medicine and pediatrics at LSU Health Shreveport.