BREAST CANCER
SCREENING & TREATMENT
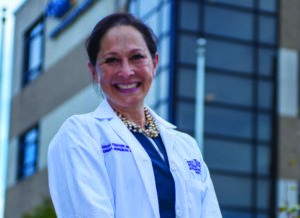
BY DR. SARAH THAYER
Breast cancer is the most diagnosed cancer among American women. Breast cancer will affect about 1 in 8, or 13%, of women in the United States. In 2021, it is estimated that 281,550 new cases of breast cancer will be diagnosed along with an additional 49,290 new cases of DCIS (non-invasive breast cancer). Breast cancer is the second leading cause of death in women with 43,600 breast cancer deaths estimated to occur in 2021. The good news is fatality rates have been steadily decreasing since 2007 and continue to decrease in women over 50. This decrease is believed to be the result of advancements in treatment and increased early detection through screening.
In the United States, the most frequent age of breast cancer diagnosis is 61 years of age. However, not everybody’s risk for breast cancer is the same. For example, African American women appear to get breast cancer at an earlier age (around 50) and have a higher rate of aggressive breast cancers. Among women 45 years of age or younger, breast cancer is more frequently identified in African American women than Caucasian women. Unfortunately, African American women are also more likely to die of breast cancer. The reason for this is unclear, but likely due to a combination of social, economic and genetic factors. Regardless of race, each woman should understand her personal risk for developing breast cancer. This depends on may factors, but can include your personal history, family history for cancer and lifestyle choices. One of the most powerful indicators for risk of breast cancer is your family’s history of breast and ovarian cancer. Approximately 15% of breast cancer cases are associated with an inherited gene that increases your risk of breast cancer.
Screening
The purpose of breast cancer screening is to decrease breast cancer mortality and morbidity through early detection. The cornerstone of breast cancer screening is breast mammography by 3-D tomosynthesis. Presently, some controversies exist among professional associations about when to start and how often to screen. For example, National Comprehensive Cancer Network (NCCN) recommends starting age at 40 with a screening interval of once per year. Other associations, such as the US Preventative ServicesTask Force (USPSTF) suggest a starting age of 50 with a screening interval of every two years. However, screening between the ages of 40 and 49 should be individualized based on your risks and values. Women of African American descent – given the early age onset of breast cancer – should consider starting at 40 and continue annually.
The question remains: whose screening guidelines should you use? Remember, breast cancer mortality is reduced with mammography. Mammographic screening is a tradeoff of risks and benefits, and not all women have the same risk. These screening recommendations are for women of average risk. However, it becomes hard to define “average risk,” as 85% of breast cancer cases is occurs in women with no family history of breast cancer.
Today there are many tools to assess your personal risk for breast cancer. Risk assessment models, such as the Tyrer-Cuzick Model, have been designed to calculate your lifetime risk for developing breast cancer. This model takes into consideration factors such as personal, reproductive, and family history of breast cancer to calculate your lifetime risk (LTR). Women above 20% LTR are considered high risk. Consult with your healthcare provider to choose the most appropriate screening strategy based on your personal risks and values around the age of 30-35.
Non-Modifiable
- Age
- Early menstruation (before age 12)
- Menopause after age 55
- Personal history of breast cancer or breast biopsy
- Strong family history of breast cancer
- Inherited genetic trait (BRCA 1 or 2; PALB2)
- History of radiation to the breast/chest
- Having dense breast tissue
- Having taken the hormone diethylstilbestrol (DES) during pregnancy or being the daughter of a woman who took DES while pregnant
- settings and even apply custom CSS to this text in the module Advanced settings.
Lifestyle-Related
- Obesity
- Not getting enough exercise
- Drinking alcoholic beverages
- Taking hormone replacement therapy
- Older age at first birth (after 30) or having never given birth
Diagnosing Breast Cancer
 Most breast cancers are identified by mammography and diagnosed by a core needle biopsy directed by either ultrasound or mammography. Receiving a breast cancer diagnosis can be overwhelming and filled with uncertainty. The good news is there are currently more than 3.8 million breast cancer survivors in the United States, according to the American Cancer Society. Additionally, early-stage breast cancer has a survival rate of 95%. Breast cancer treatments and outcomes have drastically changed in the last five years. This is mainly due to coordinated research efforts identifying that not all breast cancers behave the same and that treatments must be tailored to those risks. Treatments have now become very customized depending on patient characteristics such as age, personal risk, inherited risk, prior history of cancer, and prior treatments (such as radiation).
Most breast cancers are identified by mammography and diagnosed by a core needle biopsy directed by either ultrasound or mammography. Receiving a breast cancer diagnosis can be overwhelming and filled with uncertainty. The good news is there are currently more than 3.8 million breast cancer survivors in the United States, according to the American Cancer Society. Additionally, early-stage breast cancer has a survival rate of 95%. Breast cancer treatments and outcomes have drastically changed in the last five years. This is mainly due to coordinated research efforts identifying that not all breast cancers behave the same and that treatments must be tailored to those risks. Treatments have now become very customized depending on patient characteristics such as age, personal risk, inherited risk, prior history of cancer, and prior treatments (such as radiation).
Diagnosis also includes tumor size and whether the lymph nodes have been affected. The most important factor to determine treatment recommendations is the tumor’s behavior and risk – is it a high-risk tumor or a low-risk tumor? Insights into the nature of breast cancer come from tumor pathologic features such as grade (abnormality of cells), the expression of estrogen and progesterone receptors, the expression of HER2 hormone receptors, and its proliferative activity (how cells are multiplying and spreading). Recent advances in genetic testing can more accurately predict tumors that have higher risk. Most importantly, treatments must also incorporate your personal values.
Breast Cancer Treatment
 Breast cancer treatments are evolving. Breast cancer is no longer treated in isolation, but requires a network of breast-specific providers that work with one another to develop a comprehensive treatment plan. This plan should include recommendations for surgery, systemic therapies such as chemotherapy and/or hormonal therapy, and radiation approaches. An extensive family history should also be performed to determine if genetic testing for familial genes is appropriate.
Breast cancer treatments are evolving. Breast cancer is no longer treated in isolation, but requires a network of breast-specific providers that work with one another to develop a comprehensive treatment plan. This plan should include recommendations for surgery, systemic therapies such as chemotherapy and/or hormonal therapy, and radiation approaches. An extensive family history should also be performed to determine if genetic testing for familial genes is appropriate.
Feist-Weiller Cancer Center in Shreveport focuses on a patient-centered multidisciplinary approach to breast cancer treatment planning. The treatment approach to breast cancer is to remove the tumor (through surgery) and make sure that it does not return (through chemotherapy and radiation therapy). If your tumor is considered high-risk or aggressive (HER2-expressing tumors or triple negative breast cancer) giving chemotherapy first is favored in order to assess your tumor’s response to the drugs. Some tumors will have a complete pathologic response while other patients will have residual tumor. These patients may be considered for further therapies after surgery depending on how much cancer remains. New targeted and immune-based therapies can be added to improve outcomes.
Like chemotherapy, surgical management of breast cancer has also evolved. Surgical options include breast-conserving therapy (BCT), which involves a lumpectomy with radiation versus mastectomy (unilateral or bilateral). In the majority of women, breast-conserving therapy is preferred for the management of early breast cancer as it has the same overall survival as mastectomy. Bigger surgery does not equate with better outcomes. So, how do you choose between lumpectomy and mastectomy? Although lumpectomy with radiation is preferred for the majority of women, there are some patients who are not candidates for breast-conserving therapies. This is due to the extent of the tumor (a small breast and a large tumor), multifocal disease (meaning multiple areas of the breast are involved), the patient having prior radiation, risk of a contralateral tumor (patient with inherited genes for breast cancer syndromes), screening considerations, and most importantly, patient preference.
Since there are more than 3.8 million breast cancer survivors, consideration for improved cosmetic outcomes become paramount to improve psychosocial well-being of a breast cancer survivor and to enhance quality of life and body image. Because of this, surgical techniques have been developed to improve cosmetic outcomes. For patients considering mastectomy, nipple skin-sparing mastectomies (NSSM) are now proven to be safe. This type of mastectomy is done through incisions that hide the scar, creating a natural skin envelope. For women who choose BCT, new oncoplastic approaches have now been developed. These combine the principles of breast cancer surgery and plastic reconstructive techniques with the goal of complete resection of the lesion for improved cosmetic outcomes in a single definitive procedure. One example is using a breast reduction technique to remove and reshape the breast. Remember – the decision on what type of surgery is needed is guided by data and personal choice; it should be a shared decision between patient and care team.
In Conclusion
- Breast Cancer screening reduces breast cancer mortality and morbidity
- Current recommendation for screening is for women of AVERAGE risk
- When to start mammographic screening should be based on careful discussion with your health care provider to evaluate risks, benefits and choice
- Breast Cancer Treatments are becoming very individualized
- Surgical techniques have been developed to improve cosmetic outcome
- New targeted therapies have improved survival outcomes
- Once diagnosed patients should be referred to a multidisciplinary breast clinic for comprehensive evaluation and personalized treatment planning.
October is Breast Cancer Awareness Month. Sarah Thayer, MD, PhD, is the Director of Feist-Weiller Cancer Center.